.
8/25/20, “Virus’s retreat in Brazilian Amazon upends notions of herd immunity,” Washington Post, Terrence McCoy, Heloisa Traiano
………………………
8/29/20, Up to 90 percent of “positive” Covid tests are actually negative, NY Times review finds. Most carry insignificant amounts of virus and aren’t likely to be contagious.
……………………………
Aug. 17, 2020, “What if ‘Herd Immunity’ Is Closer Than Scientists Thought?" NY Times, by Apoorva Mandavilli, print edition, Section D, page 8
“Researchers are trying to figure out how many people in a community must be immune before the coronavirus fades.”
“We’ve known from the beginning how the end will arrive. Eventually, the coronavirus will be unable to find enough susceptible hosts to survive, fading out wherever it briefly emerges….
To achieve so-called herd immunity-the point at which the virus can no longer spread widely because there are not enough vulnerable humans-scientists
have suggested that perhaps 70 percent of a given population must be
immune, through vaccination or because they survived the infection.
In interviews with The New York Times, more than a dozen scientists said that the threshold is likely to be much lower: just 50 percent, perhaps even less. If that’s true, then it may be possible to turn back the coronavirus more quickly than once thought….
In parts of New York, London and Mumbai, for example, it is not inconceivable that there is already substantial immunity to the coronavirus, scientists said.
“That doesn’t happen in real life,” said Dr. Saad Omer, director of the Yale Institute for Global Health. “Herd immunity could vary from group to group, and subpopulation to subpopulation,” and even by postal codes, he said.
For example, a neighborhood of older
people may have little contact with others but succumb to the virus
quickly when they encounter it, whereas teenagers may bequeath the virus to dozens of contacts and yet stay healthy themselves. The virus moves slowly in suburban and rural areas, where people live far apart, but zips through cities and households thick with people.
Once such real-world variations in density and demographics are accounted for, the [percentage] estimates for herd immunity fall. Some researchers even suggested the figure may be in the range of 10 to 20 percent, but they were in the minority.
Assuming the virus ferrets out the most outgoing and most susceptible in the first wave, immunity following a wave of infection is distributed more efficiently than with a vaccination campaign that seeks to protect everyone, said Tom Britton, a mathematician at Stockholm University.
His model puts the threshold for herd immunity at 43 percent— that is, the virus cannot hang on in a community after that percentage of residents has been infected and recovered….
The virus may still flare up here and
there, even if its overall spread is stymied. It’s also unclear how long
someone who has recovered may be immune, and for how long.
Virus-Resistant Communities?…
Is it possible that some of these communities have herd immunity? In some clinics, up to 80 percent of people tested had antibodies to the virus. The highest prevalence was found among teenage boys.
But people at clinics are more likely to be showing symptoms and therefore more likely to be infected, said Wan Yang, an epidemiologist at Columbia University’s Mailman School of Public Health in New York. Random household surveys would probably find lower rates–but still well above the 21 percent average reported for New York City, she said.
Researchers in Mumbai conducted just such a random household survey, knocking on every fourth door — or, if it was locked, the fifth — and took blood for antibody testing. They found a startling disparity between the city’s poorest neighborhoods and its more affluent enclaves. Between 51 and 58 percent of residents in poor areas had antibodies, versus 11 to 17 percent elsewhere in the city. The lowest-income residents are packed tightly together, share toilets, and have little access to masks. “These
factors contributed to a silent infection spread,” said Dr. Jayanthi
Shastri, a microbiologist at Kasturba Hospital in Mumbai who led the
work.
But models likZAe Dr. Britton’s hint that it’s not impossible. Other researchers have suggested...that herd immunity can be achieved at rates of immunity as low as 10 or 20 percent–and that entire countries may already have achieved that goal….
.......
Sunetra Gupta, a theoretical epidemiologist at Oxford University, [in a] widely circulated interview…said that London and New York may already have reached herd immunity because of variability among people, combined with a theoretical immunity to common cold coronaviruses that may protect against the new one.
....“That could be the explanation for why you don’t see a resurgence in places like New York,” she said…. Immunity is a patchwork quilt in New York, for instance:Antibodies were present in 68 percent of people visiting a clinic in the Corona neighborhood of Queens, for instance, but in just 13 percent of those tested at a clinic in the Cobble Hill section of Brooklyn.
But another group, led by the mathematician Gabriela Gomes of the University of Strathclyde in Britain, accounted for variations within a society in its model and found that Belgium, England, Portugal and Spain have herd immunity thresholds in the range of 10 to 20 percent. “At least in countries we applied it to, we could never get any signal that herd immunity thresholds are higher,” Dr. Gomes said. “I think it’s good to have this horizon that it may be just a few more months of pandemic.”
Other experts urged caution, saying
these models are flawed, as all models are, and that they oversimplify
conditions on the ground…. The new models offer food for thought, he and other experts said, but should not be used to set policy. [But it already has been, is doing so right now. “Setting policy“ is exactly what the US invited a non-peer reviewed computer model to do: “A disastrously flawed Coronavirus model changed government policy overnight and shut down the world for months.” In addition to “policy,” the US rushed to use the computer model to justify transferring trillions of US taxpayer dollars. Acceptance of this computer model by Trump and his task force co-opted and trashed institutions
carefully built over hundreds of years. Americans died and were maimed
wrongly believing they were preserving these institutions. Trump also
used the computer model to justify granting of dictatorial powers to 50 US states in the name of a health emergency. Representative US government was nullified overnight simply by decree of Trump]. “Mathematically, it’s certainly possible
to have herd immunity at these very, very low levels,” said Carl
Bergstrom, an infectious disease expert at the University of Washington
in Seattle. “Those are just our best guesses for what the numbers should
look like.”…
But what about immunity at levels lower than those needed for herd immunity?
“Definitely the disease would not spread as well if it gets back into New York,” said
Joel Miller, a mathematical modeler at La Trobe University in
Australia. “The same level of behavior change will have more effect on
the disease now than it did four months ago.”
Thinking of a city or country as composed of subgroups, demarcated by age, race and level of social activity, might also help governments protect those with the least immunity.
That perspective also might help put a renewed focus on groups who require the higher levels of immunity, because of greater exposure levels and other inequities, including Black and Latino residents, said Dr. Manoj Jain, an infectious disease expert at Emory University. “That’s where this info is very useful,” he said.
The models also suggest a vaccination strategy: Rather than uniformly vaccinate all groups, governments could identify and immunize those most likely to be exposed in “superspreader” events.
“Getting those people vaccinated first
can lead to the greatest benefit,” said Dr. Michael Mina, an
immunologist at Harvard University. “That alone could lead to herd immunity.”
Vaccination schemes for other pathogens have successfully exploited this approach. For example, when children were given the pneumococcal vaccine in the early 2000s, rates of bacterial pneumonia in the elderly rapidly dropped because of a “herd effect.”…
Back in Brooklyn, fewer than 1 percent
of people tested at neighborhood clinics over the past eight weeks were
infected with the virus. But there are still handfuls of cases.”…
“A version of this article appears in print on Aug. 18, 2020, Section D, Page 8 of the New York edition with the headline: Herd Immunity Is Hard to Decipher.”
………………………………
………
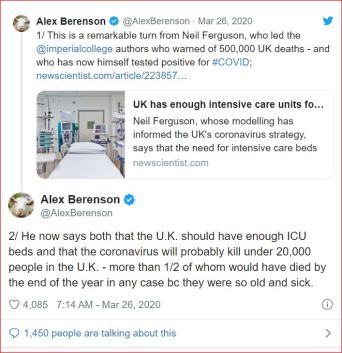
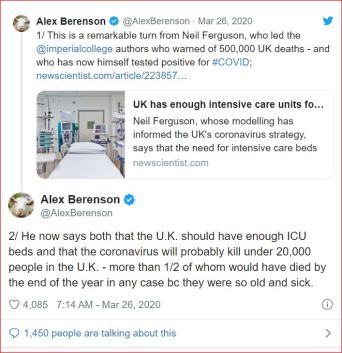
May 15, 2020, “The Lie That Launched a Thousand Lockdowns,” Dan O’Donnell, WISN1130, Milwaukee, Wisc.
“One can pinpoint the exact moment when life in the United States changed, possibly forever.
It was the night of March 11th, 2020 and the NBA suspended its season.
At about the same time, arguably the world’s most famous actor made a
shocking announcement.
The Imperial College of London projected that more than 500,000 people in Great Britain would die if no protective measures were put in place. The picture in the United States was even bleaker: 2.2 million people could die if the country didn’t close. Even with ambitious measures to mitigate the spread of the virus, the Imperial College model predicted that 1.1 million people in the United States and 260,000 people in Great Britain would die.
 [Image: 3/16/20, Trump announces 30 day virus plan, CNN, 3/17/20. UK study released on 3/16/20 predicting more than a million US deaths has not been published in a peer-reviewed journal.]
“On the guidelines of the task force, the new modeling conducted by Dr. Birx, and our consultation with governors, we’ve made the decision to further toughen the guidelines and blunt the infection now,” President Trump announced. “We’d much rather be ahead of the curve than behind it, and that’s what we are. Therefore, my administration is recommending that all Americans, including the young and healthy, work to engage in schooling from home when possible. Avoid gathering in groups of more than 10 people. Avoid discretionary travel. And avoid eating and drinking at bars, restaurants, and public food courts.”
What, precisely did President Trump mean when he referenced “new modeling” conducted by Dr. Deborah Birx, the White House’s Coronavirus Response Coordinator?
She explained later in that same press conference on March 16th.
“We have been working on models, day and night, around the globe, to really predict, because some countries are in a very early stage, like the United States,” she said. “We’ve been working with groups in the United Kingdom.
“So, we had new information coming out from a model, and what had the biggest impact in the model is social distancing, small groups, not going in public in large groups.”
That model was from the Imperial College and its chief researcher Neil Ferguson. It is hard to stress enough just how influential it was in both the U.S. and U.K., where it turned lockdown skeptics like Prime Minister Johnson and President Trump into believers overnight.
And almost overnight, states across America began implementing total shutdowns of restaurants, bars, retail stores, and every business they deemed “non-essential.”
Unfortunately, the Imperial College model on which they all relied was staggeringly, disastrously wrong.
Almost immediately after it was released, Ferguson’s model came under fire from Oxford University epidemiologist Sunetra Gupta, whose own modeling suggested that Coronavirus had been spreading in the U.K. far earlier than anyone suspected and that in most cases, it was either asymptomatic or so mild that it was confused with the common cold.
“The Oxford study is based on a what is known as a ‘susceptibility-infected-recovered model’ of Covid-19, built up from case and death reports from the UK and Italy,” The Financial Times reported. “The researchers made what they regard as the most plausible assumptions about the behaviour of the virus.
“The modelling brings back into focus ‘herd immunity’, the idea that the virus will stop spreading when enough people have become resistant to it because they have already been infected.
“If the findings are confirmed by testing, then the current
restrictions could be removed much sooner than ministers have
indicated.”
In other words, the [Neil] Ferguson model was dramatically flawed.
“I am surprised that there has been such unqualified acceptance of the Imperial model,” Gupta said.
Ferguson himself, it seems, agreed with this conclusion, because as soon as Gupta’s research was released, he walked back his doomsday predictions.
[Image: 3/16/20, Trump announces 30 day virus plan, CNN, 3/17/20. UK study released on 3/16/20 predicting more than a million US deaths has not been published in a peer-reviewed journal.]
“On the guidelines of the task force, the new modeling conducted by Dr. Birx, and our consultation with governors, we’ve made the decision to further toughen the guidelines and blunt the infection now,” President Trump announced. “We’d much rather be ahead of the curve than behind it, and that’s what we are. Therefore, my administration is recommending that all Americans, including the young and healthy, work to engage in schooling from home when possible. Avoid gathering in groups of more than 10 people. Avoid discretionary travel. And avoid eating and drinking at bars, restaurants, and public food courts.”
What, precisely did President Trump mean when he referenced “new modeling” conducted by Dr. Deborah Birx, the White House’s Coronavirus Response Coordinator?
She explained later in that same press conference on March 16th.
“We have been working on models, day and night, around the globe, to really predict, because some countries are in a very early stage, like the United States,” she said. “We’ve been working with groups in the United Kingdom.
“So, we had new information coming out from a model, and what had the biggest impact in the model is social distancing, small groups, not going in public in large groups.”
That model was from the Imperial College and its chief researcher Neil Ferguson. It is hard to stress enough just how influential it was in both the U.S. and U.K., where it turned lockdown skeptics like Prime Minister Johnson and President Trump into believers overnight.
And almost overnight, states across America began implementing total shutdowns of restaurants, bars, retail stores, and every business they deemed “non-essential.”
Unfortunately, the Imperial College model on which they all relied was staggeringly, disastrously wrong.
Almost immediately after it was released, Ferguson’s model came under fire from Oxford University epidemiologist Sunetra Gupta, whose own modeling suggested that Coronavirus had been spreading in the U.K. far earlier than anyone suspected and that in most cases, it was either asymptomatic or so mild that it was confused with the common cold.
“The Oxford study is based on a what is known as a ‘susceptibility-infected-recovered model’ of Covid-19, built up from case and death reports from the UK and Italy,” The Financial Times reported. “The researchers made what they regard as the most plausible assumptions about the behaviour of the virus.
“The modelling brings back into focus ‘herd immunity’, the idea that the virus will stop spreading when enough people have become resistant to it because they have already been infected.
“If the findings are confirmed by testing, then the current
restrictions could be removed much sooner than ministers have
indicated.”
In other words, the [Neil] Ferguson model was dramatically flawed.
“I am surprised that there has been such unqualified acceptance of the Imperial model,” Gupta said.
Ferguson himself, it seems, agreed with this conclusion, because as soon as Gupta’s research was released, he walked back his doomsday predictions.
“I should admit, we’ve always been sensitive in the analysis in the modeling to a variety of levels or values to those quantities [of people who had the virus but didn’t know it],” Ferguson told members of Parliament.
“What we’ve been seeing, though, in Europe in the last week or two is a rate of growth of the epidemic which was faster than we expected from early data in China. And so we are revising our quotes, our
central best estimate of the reproduction…something more, a little bit
above of the order of three or a little bit above rather than about 2.5.
“The current values are still within the wide range of values which…we should have been looking at previously.”
In other words, he was wrong. Spectacularly wrong. His revised projection indicated that far fewer people than initially predicted would die, and most of those who would were already so sick with underlying health problems that they would have died within a year anyway even if they never contracted Coronavirus.
On March 26th, Dr. Birx relayed this sad reality.
“I’m sure many of you saw the recent report out of the UK about them adjusting completely their needs,” she said. “This is really quite important. If you remember, that was the report that said there would be 500,000 deaths in the UK and 2.2 million deaths in the United States. They’ve adjusted that number in the UK to 20,000. So, half a million to 20,000. We’re looking into this in great detail to understand that adjustment.”
This was the first inkling Dr.
Birx or any of the government’s top disease specialists had that the
models on which they had relied were off by orders of magnitude. [But knowing this, one day later, March 27, Trump still signed a $2.2 trillion virus bailout bill which had been based on the now grossly inaccurate prediction of 1-2 million US deaths]
“We are about five times the size of Italy,” she [Birx] added. “So if we were Italy and you did all those divisions, Italy should have
close to 400,000 deaths. They’re not close to achieving that. So these are the kinds of things we’re trying to understand. Models are models. We’re adapting now to the — there’s enough data now of the real experience with the Coronavirus on the ground to really make these predictions much more sound [in the future].”
In addition, that model predicted that since Sweden did not follow the lead of the U.S. and U.K. in immediately locking down, it would have 40,000 Coronavirus deaths by May 1st. It actually recorded about 2,800.
Why was Ferguson’s modeling so flawed? He admitted that he based it on computer coding developed in 2007 to model influenza pandemics rather than Coronavirus outbreaks like SARS in 2002 or COVID-19 now.
Instead of immediately releasing that code so that it could be peer-reviewed, though, he kept it hidden for six weeks and even then only released a heavily edited version.
Sadly, this was just the latest in a long line of catastrophic mistakes from Ferguson. As National Review noted:
“Ferguson was behind the disputed research that sparked the mass culling of eleven million sheep and cattle during the 2001 outbreak of foot-and-mouth disease.”…
 [Ed. note: In 2011 a UK peer reviewed study found that slaughtering millions of healthy animals hadn’t been necessary. But, the
Queen was so impressed with Ferguson and his 2001 computer models that
called for slaughter of millions of healthy animals that in 2002 she awarded him with an OBE, Order of the British Empire. Image, 4/12/2020, “The full horrifying scale of the 2001 foot and mouth outbreak told by the Welsh farmers in the middle of it,“ walesonline.co.uk]
(continuing): “Charlotte Reid, a farmer’s neighbor, recalls: “I remember that appalling time. Sheep were left starving in fields near us. Then came the open air slaughter. The poor animals were panic stricken. It was one of the worst things I’ve witnessed. And all based on a model–if’s but’s and maybe’s.”
In 2002, Ferguson predicted that up to 150,000 people could die from exposure to BSE (mad cow disease) in beef. In the U.K., there were only 177 deaths from BSE.
In 2005, Ferguson predicted that up to 150 million people could be killed from bird flu. In the end, only 282 people died worldwide from the disease between 2003 and 2009.
In 2009, a government estimate, based on Ferguson’s advice, said a “reasonable worst-case scenario” was that the swine flu would lead to 65,000 British deaths. In the end, swine flu killed 457 people in the U.K.
So frequently and so epically did Ferguson overestimate death tolls that his colleagues mockingly call him “The Master of Disaster.”
In late March [2020], Dr. Birx recognized what British scientists did years ago: That Neil Ferguson was a hack. America needed its own modeling.
She turned to the [Bill Gates funded] University of Washington’s Institute for Health Metrics and Evaluation (IHME), which presented a model showing numbers similar to Ferguson’s: If no lockdowns were implemented, 1.5 to 2.2 million Americans would die.
If instead states kept their shelter-in-place orders going [indefinitely], though, only 240,000 people would die.
The Imperial College model was fatally flawed, but this new model was far more accurate. President Trump accepted it and on March 29th announced that “15 Days to Flatten the Curve” would be extended to the end of April.
[Ed. note: In 2011 a UK peer reviewed study found that slaughtering millions of healthy animals hadn’t been necessary. But, the
Queen was so impressed with Ferguson and his 2001 computer models that
called for slaughter of millions of healthy animals that in 2002 she awarded him with an OBE, Order of the British Empire. Image, 4/12/2020, “The full horrifying scale of the 2001 foot and mouth outbreak told by the Welsh farmers in the middle of it,“ walesonline.co.uk]
(continuing): “Charlotte Reid, a farmer’s neighbor, recalls: “I remember that appalling time. Sheep were left starving in fields near us. Then came the open air slaughter. The poor animals were panic stricken. It was one of the worst things I’ve witnessed. And all based on a model–if’s but’s and maybe’s.”
In 2002, Ferguson predicted that up to 150,000 people could die from exposure to BSE (mad cow disease) in beef. In the U.K., there were only 177 deaths from BSE.
In 2005, Ferguson predicted that up to 150 million people could be killed from bird flu. In the end, only 282 people died worldwide from the disease between 2003 and 2009.
In 2009, a government estimate, based on Ferguson’s advice, said a “reasonable worst-case scenario” was that the swine flu would lead to 65,000 British deaths. In the end, swine flu killed 457 people in the U.K.
So frequently and so epically did Ferguson overestimate death tolls that his colleagues mockingly call him “The Master of Disaster.”
In late March [2020], Dr. Birx recognized what British scientists did years ago: That Neil Ferguson was a hack. America needed its own modeling.
She turned to the [Bill Gates funded] University of Washington’s Institute for Health Metrics and Evaluation (IHME), which presented a model showing numbers similar to Ferguson’s: If no lockdowns were implemented, 1.5 to 2.2 million Americans would die.
If instead states kept their shelter-in-place orders going [indefinitely], though, only 240,000 people would die.
The Imperial College model was fatally flawed, but this new model was far more accurate. President Trump accepted it and on March 29th announced that “15 Days to Flatten the Curve” would be extended to the end of April.
The National Review’s Andrew McCarthy charted the swings: “In a space of just six days starting April 2, two revisions (on April 5 and 8) have utterly discredited the model produced by the [Bill Gates funded] University of Washington’s Institute for Health Metrics and Evaluation. I wrote about the IHME’s modeling at National Review on Monday, the day after the first revision–which was dramatic, but pales in comparison to Wednesday’s reassessment. This was not immediately apparent because the latest revision (April 8) did not include a side-by-side comparison, as did the April 5 revision. Perusal of the new data, however, is staggering, as is what it says about government predictions we were hearing just days ago about the likelihood of 100,000 deaths, with as many as 240,000 a real possibility. As I noted in my last post on this subject, by April 5, the projection of likely deaths had plunged 12 percent in just three days, 93,531 to 81,766. Understand, this projection is drawn from a range; on April 2, IHME was telling us cumulative COVID-19 deaths could reach as high as approximately 178,000. The upper range was also reduced on April 5 to about 136,000. On April 8, the projected cumulative deaths were slashed to 60,145 (with the upper range again cut, to about 126,000). That is, in less than a week, the model proved to be off by more than 33 percent.” The day after that report was published, on April 9th, FOX News anchor Martha McCallum asked the federal government’s top infectious disease expert, Dr. Anthony Fauci, about it. His answer was revealing: “I am and will always be somewhat reserved and skeptical about models because models are only as good as the assumptions you put into the model. Those assumptions that start off when you don’t have very much data at all or the data you have is uncertain, that you put these assumptions in and you get these wide ranges of calculations of what might happen. 100,240,000 deaths. But then as you start to accumulate data, likely being influenced heavily by the mitigations that you put in, physical separations, when real data comes in, then [actual] data always trumps any model. Have to modify the model and the assumptions as you get data. I have no problem with people who are critical of modeling because modeling is inherently an imperfect science. So I don’t really have any quibbling with that. You have to make sure you collect real data, you rely more on the data than the model.”
Governments apparently didn’t, as they kept citizens locked down even as the IHME model was revised again and again as it kept swinging and missing in its projections over the next three weeks.
So conspicuous were these constant alterations that Vox.com published a lengthy critique of it on May 2nd entitled “This coronavirus model keeps being wrong. Why are we still listening to it?”
“The model first estimated in late March that there’d be fewer than 161,000 deaths total in the US; in early April, it revised its projections to say the total death toll through August was “projected to be 60,415” (though it acknowledged the range could be between 31,221 and 126,703).
One analysis of the [Bill Gates funded] IHME model found that its next-day death predictions for each state were outside its 95 percent confidence interval 70 percent of the time — meaning the actual death numbers fell outside the range it projected 70 percent of the time.
This track record has led some experts to criticize the model.
“It’s not a model that most of us in the infectious disease epidemiology field think is well suited” to making projections about Covid-19, Harvard epidemiologist Marc Lipsitch told reporters.”
Three days after that stinging rebuke of the IHME model was published, the author of the Imperial College model proved once and for all what he really thought about the necessity of lockdowns.
Neil Ferguson, who had himself contracted Coronavirus in March, was forced to resign his government post after he was caught breaking quarantine to have trysts with his married mistress.
“I accept I made an error of judgment and took the wrong course of action,” Ferguson said in a statement. “I have therefore stepped back from my involvement in the Scientific Advisory Group for Emergencies [SAGE, a UK group that advises the UK government]. [4/27/20, “The government’s secret science group [SAGE] has a shocking lack of expertise,” UK Guardian, Anthony Costello. “SAGE has no molecular virologists, immunologists or intensive care experts. This could have cost thousands of lives.“]
“I acted in the belief that I was immune, having tested positive for coronavirus, and completely isolated myself for almost two weeks after developing symptoms,” he added. “I deeply regret any undermining of the clear messages around the continued need for social distancing to control this devastating epidemic. The Government guidance is unequivocal, and is there to protect all of us.”
Ferguson was the man most responsible for that government guidance, not just in the U.K., but across the globe. If the man known as “Doctor Lockdown” didn’t himself truly believe lockdowns were needed, then were they?
More importantly, why were the world’s lockdowns all premised on government models from both Ferguson and the University of Washington that have proven to be totally, completely wrong?”
………………………………………………
Added: UK issues 9000 fines for lockdown violations:
As of April 30, 2020, “More than 9,000 fines have been issued in England and Wales for breaching coronavirus lockdown restrictions.”
……………………………
Added: Ferguson was a regular “expert” guest on BBC even while he was defying UK lockdown rules:
May 5, 2020, “How Neil Ferguson, the architect of lockdown, was brought down by failing to obey his own rules,” UK Telegraph,
“Soon [after his Covid quarantine] he [Ferguson] was back to warning people, again though Twitter, about new developments in the science from his team at Imperial College. It was not good news. “Our latest estimates suggest that the virus is slightly more transmissible than we previously thought,” he tweeted on March 26.
Yet four days later [March 30] the professor was feeling well enough to break his own advice to the public and allow his girlfriend, Antonia Staats, to cross London for a visit. The following week [early April] she made a second visit to Prof Ferguson’s flat, despite telling friends she suspected that her husband had coronavirus symptoms. There is no suggestion Ms Staats visited him during the period he was
self-isolating with the virus. But to some, the tryst shows a
staggering hypocrisy and wilful flaunting of lockdown laws. Prof Ferguson sat on the Scientific Advisory Group for Emergencies (Sage), which has played a central role in advising the Government throughout the pandemic, as well as the New and Emerging Respiratory Virus Threats Advisory Group (Nervtag), which advises Dr Jenny Harries, the deputy chief medical officer, and Matt Hancock, the Health Secretary…. The 51-year-old epidemiologist [Ferguson] is married with a son but it is understood that he and his wife live apart. He is said to have met Ms Staats through the online dating site OkCupid more than a year ago…. She is a senior campaigner at Avaaz, a global online activist network
which has been praised by Gordon Brown, Tom Watson, Martin Schulz, the
president of the European Parliament, and Al Gore. She delivered a
petition to Downing Street that called for an end fossil fuel subsidies to Downing Street during the coalition government and has campaigned against Brexit….
Over the next eight days he continued to appear on the programme, and on April 4 told listeners: “Clearly we want to move to a situation where, at least by the end of May, we can substitute less intensive measures for the current lockdown we have now…I don’t think anyone wants to lift measures at the current time [April 4] and risk the epidemic getting worse.”
Yet on April 8 Ms Staats was once again at his flat. The contradiction in what he said in public and did in private did not seem to bother the professor, for on April 10, again speaking on the Today programme, he said: “We clearly don’t want these measures to continue any longer than is absolutely necessary.
“I mean, the economic costs, social costs, personal and health costs are huge, but we do want to find a set out policies which maintain the suppression of transmission of this virus.”
On Tuesday night [May 5], Prof Ferguson admitted he had made an “error of judgment” and resigned from his SAGE role.
[Ed. note: He’s back!!! In less than a month!!!]: June 2, 2020, “Prof Neil Ferguson still influencing Government’s coronavirus plan despite resigning for breaking lockdown rules,” UK Telegraph, Henry Bodkin
“On Tuesday [June 2], a witness revealed that Prof. Ferguson is leading a team contributing to one of the most influential SAGE sub-committees.”
“Professor Neil Ferguson is still influencing the Government’s coronavirus response, despite having resigned his official position for breaking social distancing rules, it has emerged.
The disease modelling expert, credited with convincing Boris Johnson [and the US] to embrace a draconian lockdown, relinquished his seat on the Government’s Scientific Advisory Group for Emergencies (SAGE) committee in May after The Telegraph revealed he had held trysts with his married lover during the height of restrictions.
The Imperial College London epidemiologist said at the time that he regretted undermining the Government’s message and that, as a result, he had “stepped back from my involvement in SAGE”.
..........
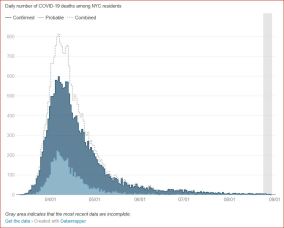 [Chart: As of 9/1/20, NYC 5 boros. Covid deaths, peaked in April, flat for 4 months. “Confirmed deaths,” 80%-89% of deaths had co-morbidities]
[Chart: As of 9/1/20, NYC 5 boros. Covid deaths, peaked in April, flat for 4 months. “Confirmed deaths,” 80%-89% of deaths had co-morbidities] 


No comments:
Post a Comment